NSoR 6: The Medicine of Religion

An excerpt from Chapter 6 of The New Sciences of Religion: Exploring Spirituality from the Outside In and Bottom Up (Palgrave Macmillan, 2010) Pages 127 – 129.
The correlations between religion, spirituality, health, and healing are ancient and modern concerns. Recent observational studies indicate a significant, mostly positive connection between religiosity and better health, though it would be difficult to isolate what aspect of religion and spirituality plays the significant role. Is it a matter of improved lifestyle, more social support, better psychological coping, positive attitudes, or perhaps something in the beliefs and rituals themselves? We now have plausible biochemical models for how nonphysical, psychosocial effects can influence the brain chemistry and the immune system. Experimental studies are much more difficult in the case of religiosity and health but, in certain limited cases, can be constructed.
I have emphasized a pervasive psychosocial somatic dimension of all healing practices, whether they be modern scientific therapies, prayer interventions, or alternative therapies. In closing, I want to argue that these psychosocial somatic dimensions are not isolated in the mind-brain-bodies of the patients but distributed through the cultural context of a society. Recent research on the social contagion of health habits and behavioral diseases strongly supports this conclusion, though without clarity about the mechanism by which psychosocial-behavioral-somatic contagion occurs.38
Placebos are encoded by cultures; otherwise. they would not exist in patients’ mind-brain-bodies. There is a culture of modern scientific medicine that encodes the popping of pills as effective placebos, along with white coats, stethoscopes, and the examination room as symbols and liturgy in the culture of sickness and healing. This is reinforced from childhood on in the rituals of visits to doctors and pharmacists, the act of taking pills at home, ubiquitous advertisements in the media, and television medical dramas from Doctor Kildare to Gray’s Anatomy. In Chinese culture, acupuncture is similarly reinforced and encoded as effective therapy. Placebos are always culturally specific, albeit in an increasingly globalized market. We can refer to cultural encoding of placebos as the deep semiotics of health.39
The question, then, is how to improve and enhance the semiotics of health in a clinical context and in a broader cultural context. How do we better utilize the placebo effect to create better health outcomes, noting that we must do so without also selling snake-oil therapies? I imagine that one of the most interesting areas of research and clinical practice will focus on harnessing the patient’s own mental powers to create powerful endogenous transformations in her endocrine and immune systems. The wisdom of CAM and spiritual interventions is that the more elaborate the healing ritual, the more effective the placebo effect.40
CAM debunker Bausell ends his book Snake Oil Science with a curious section titled “How to Select a Placebo Therapy That Works.” Bausell writes, “If you suffer from an unrelieved chronic condition, I sincerely hope that you (or medical science, conventional or alternative) will someday discover something that will help you.” But in the mean time, try a placebo! Bausell recommends shopping around for the “best” spiritual or CAM therapies and therapists: “Once you’ve started the therapy,” he continues, “embrace it . . . with all your heart and soul.”41 Here, Bausell is affirming the ancient wisdom of the second-century physician Galen, whose strange theories dominated medical practice for over a millennium. Galen noted, “He cures most successfully in whom the people have the most confidence.” Indeed, even today after all the critical analyses and best scientific practices, it helps to have blind faith and your fingers crossed. In the next chapter, we will introduce this concept as “the second naivete.” Hope heals; ritualized hope in groups heals more effectively.
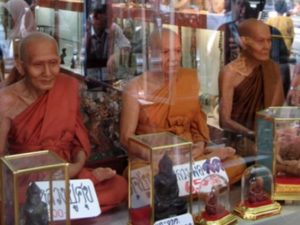
Is there a way systematically to study, ritualize, and individualize these psychosocial-somatic interventions as a supplement to the standard scientific treatments, when such treatments exist? This would require clinicians to customize the context of health care to the culture of each particular patient. An intake questionnaire might be used to provide each patient with symbols, rituals, objects, music, and care, alongside of the best medical practices, to enhance the patient’s ability to harness the placebo effect to promote healthier outcomes. For one patient, it might be a Cross by his bed and Gospel music on his iPod; for another, it might be recitations from the Qur’an and a comfortable place to perform salat; for yet another patient, it might be photographs from her pilgrimage in the Himalayas and the sound of running water, while another might want a small shrine for Lord Buddha on her nightstand and a soundtrack of chanting monks. To this we can add photographs of family and friends. New technologies make it possible to customize the spiritual-clinical environment with an infinite variety of scriptures, poems, music, images, and videos, even in a crowded hospital context. If the placebo effect is so powerful, then we should be trying to harness it to realize better health outcomes.
The Magic of Medicine
The late psychiatrist Thomas Szasz was a fierce critic of what he saw as the new religion of modern science, especially in the field of medicine, particularly in psychiatry. Szasz understood the men in white coats to be a new secular priesthood, writing, “[F]ormerly, when religion was strong and science weak, men mistook magic for medicine; now, when science is strong and religion weak, men mistake medicine for magic.”42 The most important take-away from this discussion of the medicine of religion is that there has always been, and I venture always will be, a bit of magic in the practice of medicine. All health and healing are partially psychosocial-somatic in universal and unpredictable ways. Psychosocial-somatic effects are in part instances of top-down causation in which “spirit” acts on mind, mind acts on brain, brain acts on body, and body acts on disease through the endocrine and immune systems. Religion, in this view, is an attempt to take conscious control over this dynamic. Psychosocial-somatic healing and the semiotics of health are examples of a nonreductive and functional dimension of religion and spirituality. All people and philosophies are implicated in this dynamic, which we increasingly understand in scientific causal pathways.
Practitioners of modern scientific medicine need to become self-critical in recognizing this deep semiotics of health, including in their own culturally encoded context, and become proactive in ethically harnessing these psychosocial-somatic therapies in promoting the well-being of their patients, themselves, and their societies. The medicine of religion is minimally this deep semiotics of health, from which we cannot extract ourselves, even in the practice of modern scientific medicine. This material semiosis of health — spirit-mind-brain-body-society — is traditionally the domains of religion, where significant expertise has been accumulated over the millennia. Through the medicine of religion and the tools of modern science, we might learn how better to harness this “magic” in creating better health outcomes for our patients and ourselves.
Notes
38. See N.A. Christakis and J.H. Fowler. Connected: The Surprizing Power of Our Social Networks and How They Shape Our Lives. (New York: Little, Brown and Company, 2009); Thompson, C. (2009, 9/10/2009). Are Your Friends Making You Fat? Sunday Magazine Retrieved 9/10/2009, from http://www.nytimes.com/2009/09/13/magazine/13contagion-t.html?ref=magazine
39. See Anne Harrington, The Cure Within: A History of Mind-Body Medicine (New York: W.W. Norton, 2008); Anne Harrington et al., “The Science of the Placebo: Toward an Interdisciplinary Research Agenda” (Bethesda, MD: NIH, 2000) a conference hosted by NIH in 2000, see http://placebo.nih.gov; and Harrington, The Placebo Effect.
40. T. J. Kaptchuk et al., “Sham Device V Inert Pill: Randomised Controlled Trial of Two Placebo Treatments,” British Medical Journal 132, no. 7538 (2006) 391-397.. A.J.M. de Craen, PJ Roos, and et.al., “Effect of Colour of Drugs: Systematic Review of Perceived Effect of Drugs and of Their Effectiveness,” British Medical Journal 313, no. 7072 (1996).
41. Bausell, Snake Oil Science, 291-94. v Thomas Szasz, The Second Sin (Garden City, NY: Doubleday, 1974), 128.